Prehabilitation is the name given to a programme of different activities, such as exercise, diet, and psychological support. It is designed to help an individual be better prepared, physically and emotionally, for a major event such as cancer treatment. However, the scientific evidence to support its use before cancer treatment is mixed, and the detail of what a prehabilitation programme involves if often not well explained.
Patients’ views on how prehabilitation is delivered vary, and little is known about what patients want from these services. Despite these uncertainties, many areas of the NHS recommend and provide prehabilitation for patients awaiting cancer surgery. Some of these are run across a whole city or region, but many are very small and limited to a particular hospital or even particular types of cancer. Different services are available to different people in different parts of the country, with some people having no suitable services available at all.
We aim to make a major contribution towards addressing the problem of variation in prehabilitation before cancer surgery. We will work with patients, carers and healthcare professionals to find ways to describe, measure and assess the quality of services. We will also identify and share examples of best practice about how services are developed, funded and delivered. This project answers the call made by the NIHR, Royal College of Anaesthetists and Macmillan to “gather examples of how local areas have had prehabilitation commissioned as part of the cancer pathway”.
People from underserved and minority backgrounds often have poorer health outcomes and prehabilitation has the potential to worsen inequalities, which may mean that it works better for some than others. For example, some people may find it harder to engage with prehabilitation because of limited access to exercise facilities, the internet, transport, funding and time. This project will specifically aim to describe the ways in which prehabilitation is affected by health inequalities, and capture any solutions developed to address them and make services more equitable.
The project has four main parts:
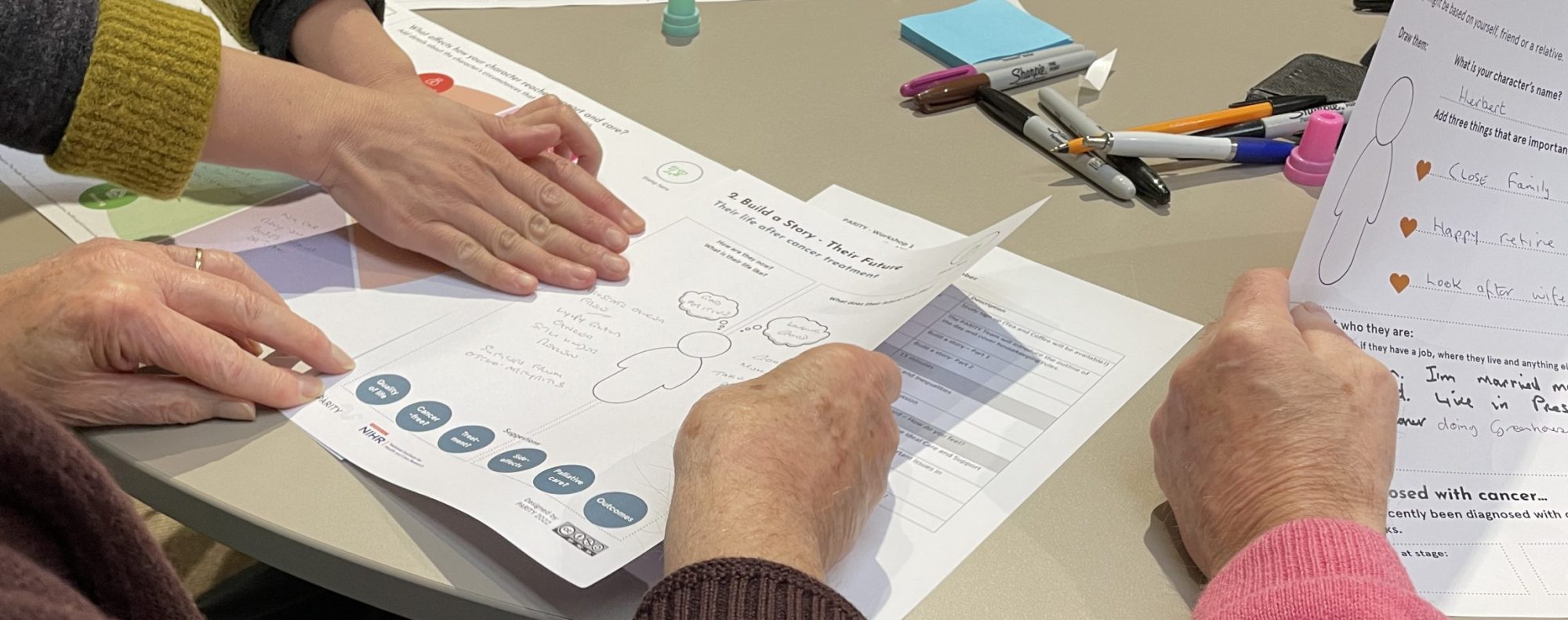
1. Defining aims, objectives and values: we will work with patients, clinicians and researchers to codevelop criteria that explain what is important about prehabilitation, in order to describe and evaluate services.
2. Mapping: making use of the co-developed criteria, we will produce a national map of prehabilitation services. This will also record data about how services are funded, who delivers them, and how they are delivered.
3. Case studies: using the national map, we will identify 8 services for in-depth analysis through observations and interviews with patients, carers and staff. This will allow us to identify areas of best practice.
4. Informing policy and practice: drawing on the results of the project, we will produce a set of best practice principles for prehabilitation prior to cancer surgery. We will also make the national map available as a resource for others to use.